Summer is here! And with it, big running efforts. Whether you’re training for that local 5K or your first ultra, many athletes are ramping up their mileage.
Consequently, it means the season for runner’s knee—also known as patellofemoral pain syndrome (PFPS). We’re going to break down the causes of that knee pain and map out solutions to get your knees in check and your running plans back in motion.
Biomechanics of the knee
Let’s take a moment and review what a knee is and why it’s susceptible to pain during and after endurance activities.
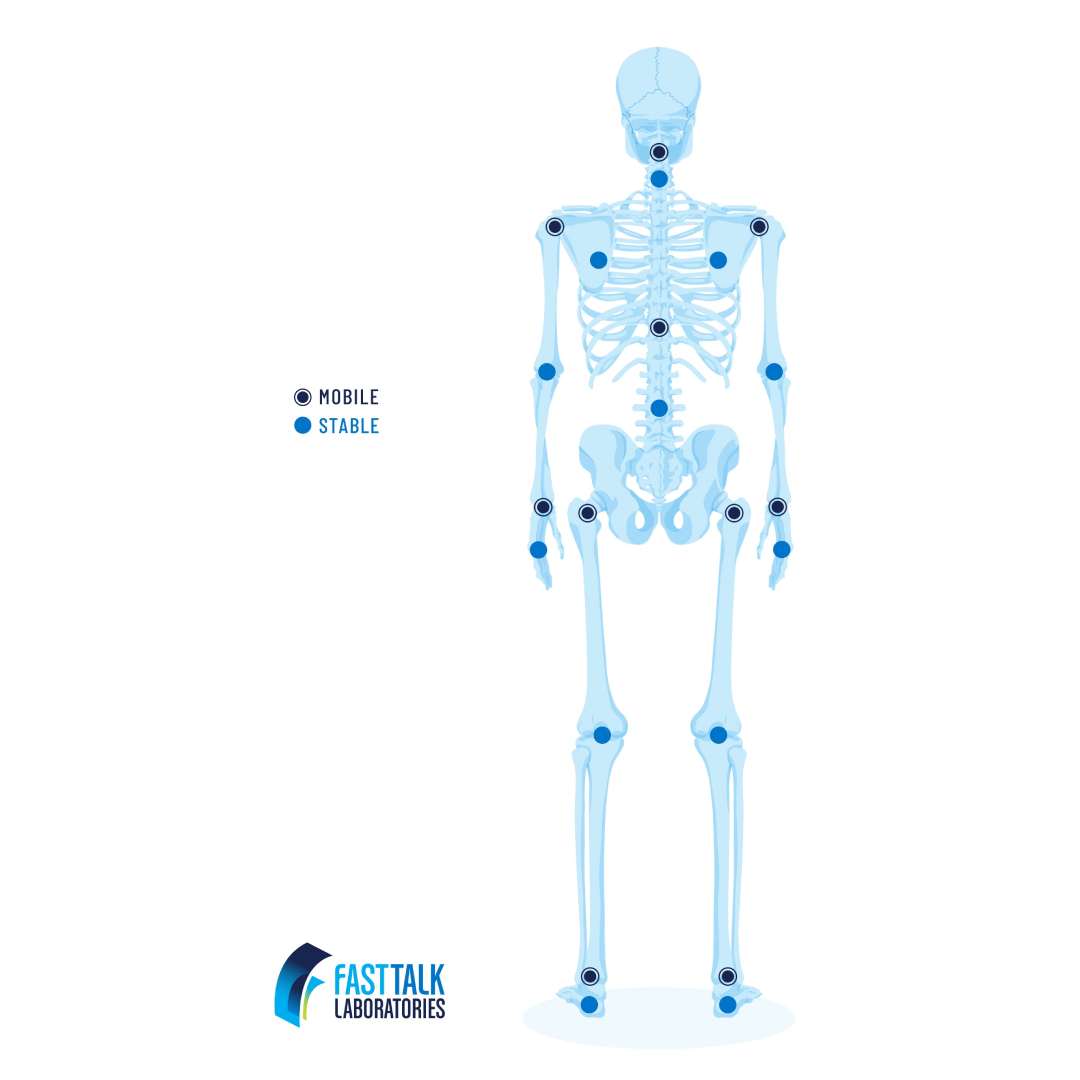
First off, let’s think about how the joints in your body work. In general, joints alternate from being more mobile (moving in many directions) to more stable (having one or two primary movements). The knee’s primary job is to flex and to extend, and it sits smack between your very mobile ankle and your very mobile hip. [1] Because of that, your knee is extremely reliant on your ankle and hip being strong and safe—it’s just along for the ride.
Zooming in more, we know the femur articulates with the tibia, and above the femur is the patella, which floats above and connects to the system via the quadriceps and patellar tendons. To flex your knee, both static and dynamic structures need to perform in order to keep your joint aligned and happy throughout the movement. [2]
Your patella acts like a pulley system for your quadriceps, particularly as you go from a flexed position to a completely extended leg. [2] As your knee straightens, your patella drifts superiorly—that is, upward—to facilitate the motion. If you don’t have 10mm of motion as you go from a relaxed, extended knee to a contracted quadriceps, there’s potential for pain. [2]
What is runner’s knee?
Simply put, runner’s knee describes poorly localized pain around the knee joint, and it typically increases in severity the more your knee is loaded or flexed. If you see a healthcare provider about it, they will likely call it PFPS. The most common areas to experience this pain is underneath the kneecap (anterior retropatellar) or in and around the kneecap (peripatellar). [1]
It can feel frustratingly non-specific to get a PFPS diagnosis. Some athletes can get a spike in knee pain immediately following a tough effort, while some might notice a building of anterior knee pain as they increase their mileage from week to week.
How to treat runner’s knee
The first step to treating PFPS is by determining what type of subcategory your knee falls into. These categories are not meant to silo your treatment—you can benefit from interventions related to all four—but understanding which subtype is most aligned with your presentation can inform your timeline for recovery.
- Overuse/overload without other impairment. This is a likely category to fall into as a distance runner. If you are loading your knee without enough rest, the tissue in your knee will likely respond. You might present with some light edema (swelling) to the joint, and uphills or downhills likely aggravate your symptoms.
- Muscle performance deficits. You can fall into this category if you go through muscle testing for your lower extremity and weakness or motor control deficits are noted in your posterolateral hip musculature, hip flexors, quadriceps, or hamstrings.
- Movement coordination deficits. This category usually presents as chronic irritation to the knee tissues from repetitive, adverse movement patterns. We typically see excessive hip drop and the knee “collapsing” inward with impact. Gait and movement retraining is the usual first step in intervention.
- Mobility impairments. If you have a substantial limitation in your hamstrings, quadriceps, triceps surae complex (calves), lateral retinaculum (outer side of knee), or IT band, the pull on your kneecap can be altered. This mobility deficit will cause your patella to not “track” well as you load your knee.
Regardless if you’ve seen a medical provider to treat your pain, there are some catch-all solutions that can improve your symptoms.
RELATED: How to Bulletproof Yourself Against Plantar Fasciitis
Step 1: Control the swelling
Studies have shown that a slight edema in and around your infrapatellar fat pad (think pillows that help cushion your knee around each tendon) results in a significant decrease in the ability to generate force as you straighten your knee (particularly 120-180 degrees, with 180 being totally straight). [3]
More so, the contact area between your patella and the underlying femur is substantially reduced with only a trace amount of swelling—and the amount of stress placed on the patellofemoral joint is dependent on the surface area of the patella in contact with your femur (i.e., the more contact, the less stress). PFPS is primarily stress caused to the joint. [4]
The solution is simple: Two to three times a day, elevate your knee so that it’s above your heart. For 15 minutes (particularly after activity or toward the end of your day), put ice on your knee.
The way we get fluid back to our hearts from our legs is with a one-way muscular valve system in our calves. So do some ankle movements or pumps to activate your calf during this time and help “flush” your knee more effectively.
Short on time? Take an ice cube from the fridge and massage the area that causes you pain. Let it completely melt.
Step 2: Deload
When a joint is in pain, your ability to voluntarily activate that tissue appropriately diminishes. In other words, your quadriceps, hamstrings, and gastrocnemii (largest parts of the calves) all present “weaker” when you’re in pain, and you subconsciously begin compensating. [4]
The first step is to not reinforce your new compensatory motor strategies. No one wants to hear this, but you need to avoid activity that causes pain above a 3 out of 10. Start by taking 48 hours off from that type of activity and reassess.
Step 3: Reload
The most essential muscles you need to retrain to activate are your gluteus medius (remember, the knee is subject to the hip and the ankle!) and your vastus medialis oblique (your inner quadriceps muscle). [2] Try these exercises, focusing on motor control but keeping your pain at 0 or 1/10. If something really flares your symptoms, talk to a physical therapist. Some discomfort is okay but try to stay close to pain-free during your reloading stage.
1. Side Lying Hip Abduction
Find your gluteus medius, isolate it, and activate it! The muscle supplies stability to your pelvis, and it’s correlated to your quadriceps function and ability to load your knee safely in high impact activities. [4] The key to motor control is repeating the motion correctly and frequently. Consider doing 2-3 sets of 10-15 repetitions (or until you feel your muscle burn) and repeat twice a day.
2. Side Plank
Now you’re working on loading your posterolateral hip musculature and your obliques while in a closed chain position. This is a great way to bulletproof multiple joints at the same time. Try 3 sets of 20 seconds, focusing on keeping your hips stacked the entire time.
3. Single Leg Squat with Isometric Hop Abduction
Time to put the building blocks together by loading in a functional position. Watch yourself in the mirror as you slowly bend and straighten your standing leg. Don’t let your kneecap dip inward during this motion. Do not do more than you can comfortably do with your hip musculature turned on and your kneecap facing forward.
4. Quad-Specific Strength Exercises
For this, there are a lot of options. You need strong quads to support your knee, but you need to start with pain-free knee exercise. This might initially mean something that should make your brain sweat more than your body: quad sets. Remind your quadriceps how to fire in a non-painful way. Start with contracting your quads only as much as is comfortable for your knee. Try 3 sets of 20 reps spread throughout your day.
5. Foam Roll
You also should address any mobility limitations you have—the most common being tightness in your lateral compartment (IT band and lateral reticulum, aka the outer kneecap) that could be causing your patella to be pulled up and out. [2] Consider rolling the outside of your hip, your tensor fascia latae (upper outer thigh), and your vastus lateralis (one of your quadriceps). There are other ways you can focus in on your mobility, but start here.
RELATED: The Athlete’s Guide to Foam Rolling
Following these steps is the best way to start solving your knee pain. If your pain persists, talk to your local PT!
References
[1] Willy RW, Hoglund LT, Barton CJ, Bolgla LA, Scalzitti DA, Logerstedt DS, Lynch AD, Snyder-Mackler L, McDonough CM. Patellofemoral Pain. J Orthop Sports Phys Ther. 2019 Sep;49(9):CPG1-CPG95. doi: 10.2519/jospt.2019.0302. PMID: 31475628.
[2] Loudon JK. Biomechanics and Pathomechanics of the Patellofemoral Joint. Int J Sports Phys Ther. 2016 Dec;11(6):820-830. PMID: 27904787; PMCID: PMC5095937.
[3] Kim EK. The effect of gluteus medius strengthening on the knee joint function score and pain in meniscal surgery patients. J Phys Ther Sci. 2016 Oct;28(10):2751-2753. doi: 10.1589/jpts.28.2751. Epub 2016 Oct 28. PMID: 27821928; PMCID: PMC5088119.
[4] Bohnsack M, Klages P, Hurschler C, Halcour A, Wilharm A, Ostermeier S, Rühmann O, Wirth CJ. Influence of an infrapatellar fat pad edema on patellofemoral biomechanics and knee kinematics: a possible relation to the anterior knee pain syndrome. Arch Orthop Trauma Surg. 2009 Aug;129(8):1025-30. doi: 10.1007/s00402-006-0237-z. Epub 2006 Oct 13. PMID: 17053945.
[5] Tayfur B, Charuphongsa C, Morrissey D, Miller SC. Neuromuscular Function of the Knee Joint Following Knee Injuries: Does It Ever Get Back to Normal? A Systematic Review with Meta-Analyses. Sports Med. 2021 Feb;51(2):321-338. doi: 10.1007/s40279-020-01386-6. PMID: 33247378; PMCID: PMC7846527.




