Most of us have heard the term “plantar fasciitis” (PF), and it’s usually in the context of a frustrated friend (or yourself!) complaining about nagging, irritable pain on the bottom of their foot that seems to last forever.
It turns out that one out of every 10 Americans suffers from chronic pain on the bottom of their foot, and 8-22% of athletes get plantar pain at some point. [1]
RELATED: How to Bulletproof Yourself Against IT Band Syndrome
What exactly is plantar fasciitis?
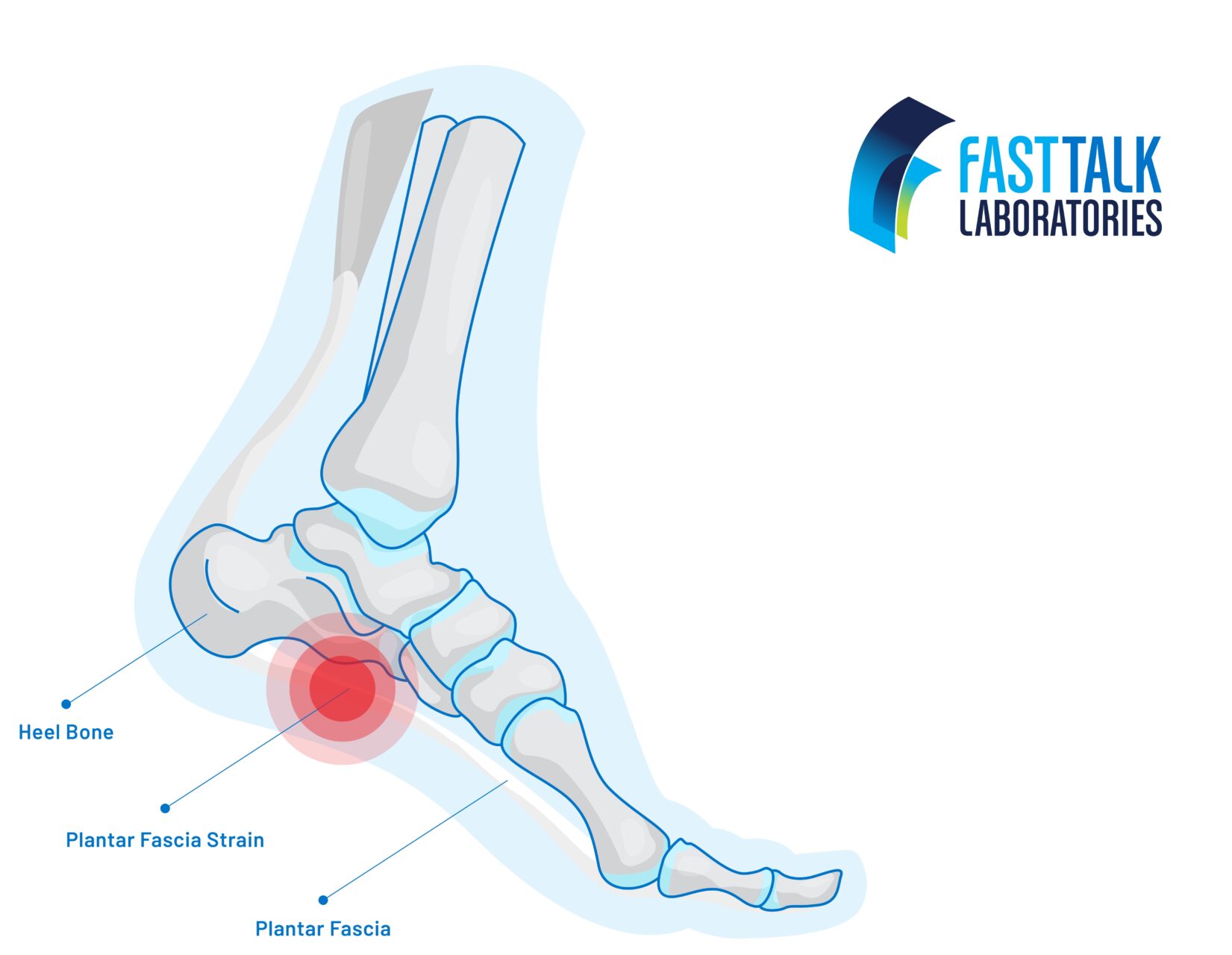
The term “plantar fasciitis” is actually not the accurate name for what’s going on. Yes, it relates to the plantar surface of your foot. But “fasciitis” implies that the fascia (connective tissue) gets inflamed (-itis). In fact, the opposite is usually happening: there aren’t inflammatory cells present, so we should be calling this condition “plantar fasciosis” to indicate that this is a degenerative condition. [2]
Plantar fasciitis symptoms
First off, if you notice your first few steps in the morning cause substantial pain that lessens as you start moving more, this could be a sign that you have the condition.
If you go to a healthcare provider, they will look for other signs and symptoms. This usually includes palpating your inside heel; if you have PF, this will be tender.
The third cardinal sign is that this pain has been bugging you for more than a year. [2] That being said, I strongly recommend not waiting a full year to start on some interventions!
Providers will also test your foot by pulling up on your big toe to “tent” your arch muscles. This is called the windlass mechanism, and it refers to how the plantar fascia creates extra stability to your horizontal longitudinal arch as you bear weight through that side. [2] There are a few other key factors that can influence a diagnosis, including an assessment of your foot posture (overpronation and high arches increase your chances of getting plantar fasciitis) and taking into account your weight (higher BMI means more pressure through the foot) and gender (women are more likely to get this). [2]
Especially considering the contentious name, I want to reiterate that an official diagnosis isn’t necessary to begin some gentle therapeutic exercise and manual therapy that could improve your symptoms.
Before we go on, let’s be clear: There are many other conditions that can affect pain on the bottom of your foot. It’s a good idea to check in with your PT to try to home in on your diagnosis, especially if it’s not responding to the interventions below.
RELATED: How to Bulletproof Yourself Against Runner’s Knee
How to treat plantar fasciitis
Stretching
Motion is lotion! I recommend splitting up your day to have multiple bouts of stretching. Doing 10 minutes of stretching once a day is not as effective as many, smaller stretches throughout the day. Beyond stretching the foot itself, the literature also strongly recommends stretching the gastrocsoleus complex (calf muscles). [3] I recommend holding the stretches gently and for longer—think 45-60 seconds for each.
Motor control
After finishing a round of stretching, this is the paramount next step. Without motor control and strengthening elements in your program, there’s no reason your biomechanics and loading patterns will shift—and without that, don’t expect a big change in symptoms.
Think of motor control exercises as a way to strengthen your brain’s awareness of your foot. When your body is in pain, it will light up your brain with pain signals; over time, your brain’s map of the body (called your homunculus) can get “smudged” and the painful parts of your body can feel more intense and harder to pinpoint. By going through these exercises, you can “re-chart” your homunculus and decrease your pain while improving your function. [4]
Load the tissue
Keep in mind that those who overpronate (meaning excessive foot collapse when you’re bearing weight) can have more biomechanical stress to the medial heel area, and this is a part of plantar fasciitis presentation. That means that you need to make sure you bridge the gap between motor control work and loading your tissue in a way that simulates the high-impact activity you’re trying to return to.
It’s important to take your motor control building blocks and begin loading your calf and foot progressively—and with excellent form. The videos below demonstrate good control at the ankle while you lift and lower your heel. I recommend both of these exercises (yes, even though it says it’s for Achilles tendonitis!).
If you’re wondering how your form is, start by doing heel lowers with both legs, not just one. As a bonus, put a tennis ball between your heels and lightly squeeze; this will keep your ankle “neutral” and not let the collapse take place.
Other treatment options
Orthotics
There is a lot of discussion around the effectiveness in using orthotics for this condition. The current PT guidelines indicate that you can use over-the-counter or custom orthotics with similar effect. The effect is, namely, that your pain should be somewhat alleviated in the short term. [5] In the medium term (think 2-12 weeks) and longer, the results are less clear as to whether orthotics truly improve symptoms and prevent future plantar fasciitis. [4]
How I look at it is this: there are exceptions to every rule (for instance, if your foot posture is very abnormal), but if you think about what orthotics for PF are doing, they are limiting how much your foot moves to improve your biomechanics. There are four layers of muscles—called your intrinsic foot muscles—along with your plantar aponeurosis that are there to stabilize your foot.
Use orthotics to alleviate acute symptoms, but work on your loading program to try to improve your arch control and strength so that you can transition safely away from orthotics down the line.
Kinesiology taping
Orthotics aside, taping along your arch is also recommended to improve your symptoms. Try this at-home tape job—if your foot pain improves, orthotics could be a good match for you.
Dry Needling
At this time, dry needling is not recommended. That being said, everyone is different: talk to your provider if you want to learn more about this.
If you still have questions about your foot pain, talk to your local provider or reach out to me. Happy foot strengthening!
References
- Buchanan BK, Kushner D. Plantar Fasciitis. [Updated 2022 May 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431073/
- Rhim HC, Kwon J, Park J, Borg-Stein J, Tenforde AS. A Systematic Review of Systematic Reviews on the Epidemiology, Evaluation, and Treatment of Plantar Fasciitis. Life. 2021 Dec;11(12):1287.
- David JA, Sankarapandian V, Christopher PR, Chatterjee A, Macaden AS. and Injected corticosteroids for treating plantar heel pain in adults. Cochrane Database Syst Rev. 2017; 6: CD009348. https://doi.org/10.1002/14651858.CD009348.pub2
- Evidence In Motion. O Body Part, Where Art Thou? Evidence In Motion. Published August 8, 2023. Accessed June 30, 2017. https://evidenceinmotion.com/o-body-part-where-art-thou/
- Journal of Orthopaedic & Sports Physical Therapy. “Heel Pain—Plantar Fasciitis: Revision 2014.” Journal of Orthopaedic & Sports Physical Therapy, vol. 44, no. 11, 31 Oct. 2014, pp. A1-A33. DOI: 10.2519/jospt.2014.0303.




