This episode marks a big moment for Fast Talk! This is our first episode with Rob Pickels as our new co-host.
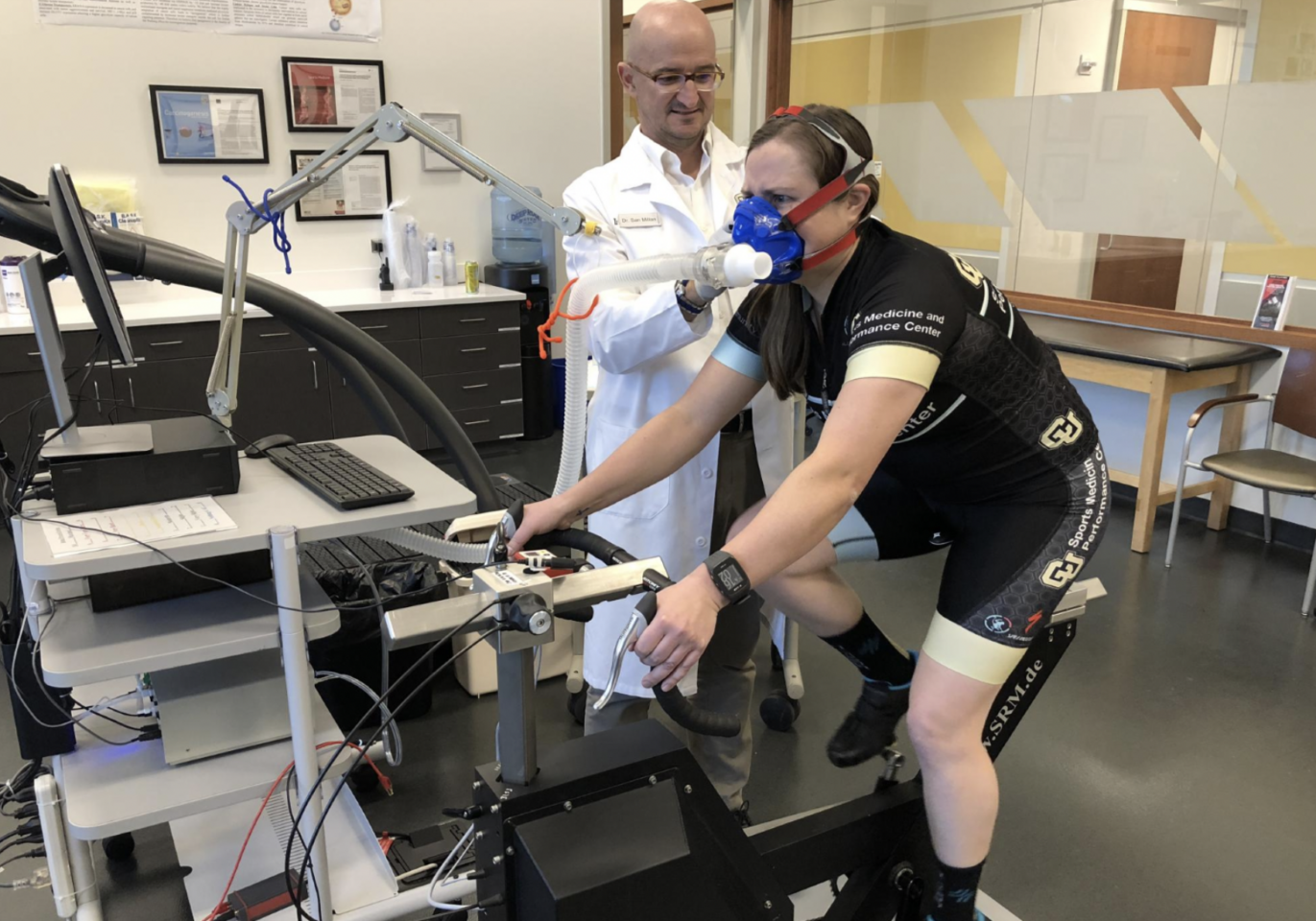
For Rob’s first episode, we brought in a very special guest: Dr. Iñigo San Millán. The two of them worked together at the University of Colorado’s Sports Medicine and Performance Center. Dr. San Millán is the head physiologist for UAE Team Emirates, and coaches 2021 Tour de France winner, Tadej Pogačar. But since winning the Tour de France wasn’t enough for him, he’s also doing work with Dr. George Brooks on the role of lactate metabolism in cancer.
You’ve heard us say it a hundred times before: if you want to be at your best, you have to take your recovery seriously. In this episode, Dr. San Millán dives into the physiology of why we need recovery. He explains cortisol, catabolic states, the breakdown of muscle protein, and why staying in a catabolic state not only can lead to overtraining, but also chronic inflammation and even disease.
Dr. San Millán recently wrote a paper on the biomarkers of recovery, and we finish out the episode by offering suggestions on the ways you can test and monitor your recovery. So, in short, our message for today is get your rest.
Joining Dr. San Millán, we hear from a host of other experts including Dr. Jason Glowney, who was the head physician at CU Sports; Armando Mastracci, the founder of Xert training software; and coach Jeff Winkler here in Boulder.
So, sit down, strap on your compression boots, check your cortisol levels, and let’s make you fast!
Episode Transcript
SPEAKERS
Dr. San Milan, Trevor Connor, Rob Pickels, Jeff Winkler, Armando Mastracci, Dr. Jason Gladney
Intro
Trevor Connor 00:04
Hello and Welcome to Fast talk your source for the science of endurance performance. I’m your host Trevor Connor. This episode marks a big moment for Fast Talk. This is our first episode with Robert Pickels as my new co host of excited to have him as part of the team. I really can’t wait to see what he brings to the show and got to admit now I’m really gonna have to keep on top of my research because Rob knows his stuff. For Rob’s first episode, we brought in a very special guest Dr. Inigo San Milan the two of them work together at the University of Colorado Sports Medicine and Performance Center. Dr. San Milan is the head physiologist for UAE Team Emirates and coaches 2021 Tour de France winner Tadej Pogačar, but since winning the Tour de France wasn’t enough for Dr. San Milan he’s also doing work with Dr. George Brooks on the role of lactate metabolism and cancer. You’ve heard us say it 100 times before. If you want to be at your best you have to take your recovery seriously. In this episode, Dr. San Milan dives into the physiology of why we need recovery. He explains cortisol, catabolic states, the breakdown of muscle protein and why staying in a catabolic state can only lead to overtraining but chronic inflammation and even disease. Dr. San Milan also recently wrote a paper on the biomarkers of recovery and we finish out the episode by offering suggestions on ways you can test and monitor your recovery. So it’s short. Our message today is get your rest joining Dr. San Milan we hear from a host of other experts, including Dr. Jason Glowney, who was the head physician at CU Sports, Armando Mastracci, the founder of Exert training software, and coach Jeff Winkler here in Boulder. So sit down, strap on your compression boots, check your cortisol level, and let’s make it fast.
Rob Pickels 01:48
On last week’s episode number 204. We said farewell to our longtime co host, Chris case. He’s back this week, in a sense as we share Chris’s N1 challenge video on fasttalklabs.com. About a year ago, the Fast Talk Labs team all declared a personal N1 challenge, a big scary ride that would push each of them to test themselves to try something new and to push their limits. Chris Case’s then one challenge was bikepacking around an entire country, the island nation of Iceland. Our video producer Sam Sullivan has released Chris’s N1 challenge video on our website. Watch as Chris and a partner ride past spectacular coastlines, roaring waterfalls and blasting volcanic sand storms over epic 200 Kilometer days in the saddle and nights spent under the stars. If you thought you knew Chris Case, think again. Watch his new N1 challenge video for an all new appreciation of Chris who embodies cycling grit and a love of exploration. See it at fasttalklabs.com.
Trevor Connor 02:55
Well, Dr. San Milan, welcome back to the show. It’s always a pleasure having you these are always great episodes with your knowledge of physiology and training and coaching. And I have to say, you know, this is kind of a special episode for us in several ways, because this is our first episode with Rob as my co host. And you too have a bit of a background with one another.
Rob Pickels 03:18
We do and I can’t believe that this is the first episode Trevor that you and I have together and then also bringing Dr. San Milan in, because I’ve worked with some absolute pillars in the sport science world. And I’m extremely fortunate to have had Dr. San Milan mentor me so I cannot share the countless things that he has taught me that I’ve learned from him. It’s really a benefit to me and a benefit to all of our listeners.
Dr. San Milan 03:42
Thank you very much, Rob for the nice words and, and Trevor, also for the invitation. It’s great to be back and I appreciate it. And Robbie, I was I was also very fortunate to be able to work with you very talented physiologist and it was always a great experience. So really appreciate it. It’s always a pleasure to be back
Dr. Iñigo San Millán Discusses How to Maintain a Healthy Workout Routine
Trevor Connor 04:03
A bit of a special episode for all of us. And like I said, it’s always a joy having you on the episode. So today we’re going to talk about not just recovery, but something I really appreciate from you is that we have all these ways of measuring training, but you’re really going to talk about the importance of being able to measure recovery. But before we get there, I have a question for you that I’m really actually excited to ask you because we’ve talked a lot of times on the show about you need recovery, recovery is important about how cyclists and endurance athletes tend to really focus on the training side, but they see taking time off the bike taking the running shoes off and sitting on the couch as loss training, which they shouldn’t see it as. So I want to ask you from a physiological standpoint, why is recovery so essential to training?
Dr. San Milan 04:51
Yeah, well so as you said very well we focus too much or the right amount of time right on training and bioenergetics and nutrition different training zones, etc. Right. But yeah, I think it’s great not to focus also on recovery, which is an area that many times is overlooked by many people out there. And it’s absolutely key, because that recovery period is we’re going to, you’re going to simulate and super compensate and many of these metabolic stressors are elicited by training, they need to be completed in the recovery phase, right? We, we have to always or I try always to keep in mind that training and competition is both physiological and metabolic, in even mental stress on the body, right and that’s what’s going to elicit multiple responses to improve. But again, you know, without proper recovery, it is not going to be possible to optimize those stressors, elicited by exercise. That’s why recovery is a big deal and at least, you know, overall, this 26 years working with athletes to knee recovery, and monitoring their recovery, as we’re going to speak about recovery is not just go and take a nap or go to sleep eight hours, right? There are many more areas, but this has been as big as training, to me at least.
Trevor Connor 06:12
So what would you say? I mean, a lot of our listeners obviously are not pros, they’re not training six hours a week and and I’ve heard this from people where they’ll say, I don’t go out and do six hour rides, I don’t train 30 hours a week, I’m just doing one, two hours. So it’s stressful, but it’s not that stressful on my body, my body can handle it. So I don’t need to take recovery days, what would your response to them be?
Dr. San Milan 06:33
Yeah, it’s like you’re right, the response will be like, you can really get over trained and fatigued, even if you train only six hours a week, or seven hours a week, and I do it myself, right? I you know, most of us are very busy with a lot going on. And we try to squeezing time from work or family or multiple things that we might be doing. And we might not be able to do more than eight hours. Right? But it is that our regular activities that might interfere with our training. So, you know, it happens to me that, you know, when when I have, for example, a very stressful week or very busy week, I might go out for an hour and have right and I’m dead tired. And that might be just my second day of the week. And like I so yeah, so that’s what I knew, like, well, how in the world I’m overtrained or fatigue, by when I’m just turned an hour and a half and last week, I only trained three days or four days, and I and not over an hour and a half any of the days. So you know, intuitively you think there’s no way I’m over trainer fatigue, but yes, you are. Because, you know, like you have so many stressors or so many things in life that interfere with your exercise, that even a small dose of exercise can be difficult to overcome.
Rob Pickels 07:46
You know, and I think when these time crunched athletes, because that’s a lot of what we’re talking about. They are viewing training as the way that they get better. And everybody is in this to improve their performance. But they’re not willing to take the recovery when they really ought to be because even if overtraining isn’t the issue, that recovery is important to the adaptation that improves their performance. So by missing out on the recovery, they’re not ultimately getting the goal that they’re working so hard toward achieving
Trevor Connor 08:16
Agree completely. – Yeah me too. – So getting ready for this podcast, Rob, and I both actually read a paper of yours that I really enjoyed. So that’s your,it’s actually a chapter called blood biomarkers and sports medicine and performance and the future of metabolomics and something I really liked in there as you you talked about overtraining, and you expressed overtraining as essentially a recovery imbalance.
Dr. San Milan 08:41
Yeah that’s how I would describe it. Right, yeah, it’s like, when someone’s over trained, there’s an imbalance there, either the input from the training dose is too much, and or the recovery is too little. And there’s like, that imbalance. And many times the stars by the training, you know, maybe that training zones are not correctly dialed in for an athlete. And we may think that say, as an example, that that athlete is training zone two, but actually is training so free, right, so if you do that multiple times a week, you’re definitely going over, you know, the prescribed zones, or sometimes, maybe the high intensity workouts, you know, like the threshold, again, it might not be very well they lean in, you’re actually going over right, or maybe just the way they’re spaced out is not enough, right? And then on the other side, is the, maybe the nutrition is not there, maybe the person is restricting carbohydrates, or maybe the nutritionist, working with that athlete is trying to get that athlete on a diet that is going to be more restrictive in calories without taking into account, but that athlete is training and therefore they’re not on the same page and that might very well cause overtraining, which is what I see so many times.
Trevor Connor 09:57
That’s interesting because Ryan Koehler head coach, he’s brought that up a lot that sometimes problems with training, problems with energy is just due to an insufficiency in nutrition.
Dr. San Milan 10:08
Absolutely and I’ve always enjoyed working with Ryan, he’s one of the best nutritionist I’ve worked with and yeah, we always were interacting together, bring in both energy balance and training workload. And yeah, we had multiple discussions and yeah, they go together, and any one of them is off is difficult. And this is why now even with, you know, the portraiture, for example, you know, like, every single day that he trains, he has his nutrition dialed in, according to the training workload, so the train the data, he trains more, or nutrition network operator, which is what, who’s one of the best in the world, he would communicate all the time. So he prescribes the nutrition according to his specific workload for today, tomorrow will be a different day. And then with different workload, so he will adjust that specifically for tomorrow’s workout. And then there might be things along the way, where maybe enough that he’s feeling tired or fatigued, or maybe not total ready, so okay, we’re going to change the workout tomorrow, and therefore, the nutrition will be changed as well, or maybe increased or so. But I think they go hand to hand nutrition and training. It’s a must. And this is something that now they’re starting to interact. But yeah, you know, not just in cycling, but in other teams, you know, you see that you know, more about the training side on one hand, and then nutrition, on the other hand, not not talking to each other. And, and this is very, very important.
How Does Overtraining Lead to Changes in an Athlete’s Body?
Rob Pickels 11:39
Now, Dr. San Milan when we’re talking about nutrition, being imbalanced with the training for you, is that a general nutrition strategy is that carbohydrate restriction, what are we seeing from athletes that’s causing the potentially to increase the risk of overtraining?
Dr. San Milan 11:56
Yeah, that’s a great question and I see that as a little bit of everything. But I think that if I were to kind of identify one element is usually carbohydrates, right? Athletes, they they don’t many athletes, they tend to restrict carbohydrates, or not have enough, we know that when you train, even at an aerobic level, riders on tour, so you can you can burn or oxidize about, 1.5 to 2.5 grams per minute. Right. So yeah, that’s a lot of carbohydrates. Although we, we normally think that this is just fat burning zones, right? But you also burn glucose, so we should not. Yeah, we should remember about that. So because those days are typical days, where an athlete says, Oh, I train aerobic I burn fat, I don’t need to eat a lot of carbohydrates. Well, we’ll actually yeah, you burn that day, maybe 300 grams of carbohydrates, or 500 grams of carbohydrates. So there, that’s right there, your entire glycogen storage is. So this is what our nutrition has to be there, and I think that carbohydrates, its main problem that we see, then that’s where when cyclists are, you know, athletic getting to this research cycle that I call because let’s say that, you didn’t say that you needed to replenish carbohydrates correctly today, but actually, you run out of glycogen storage is or we’re low. In tomorrow, you have a big day, whether it’s intensity, or whether it’s the duration, you don’t have enough carbohydrates. So you’re going to start tapping on muscle protein, because as we know, muscle protein, different amino acids, a main one is glutamine can be utilized for energy directly into the mitochondria, right? Or other gluconeogenic amino acids, like many of the branched chain amino acids can be become glucose, right? So the body has this way to try to provide your energy. But in these situations when there’s no glycogen, yeah, it’s just like, it’s like the muscles to start eating themselves to feed themselves. And that’s where you start getting into more catabolic situation and that anabolic to catabolic balance is disrupted, and that that can put any athlete right there in overtraining in no time.
Rob Pickels 14:11
Yes, certainly. You mentioned that there’s an increase in energy created from protein right through gluconeogenesis. What other downstream effects does training with low glycogen have are their endocrine system changes or anything else?
Dr. San Milan 14:26
Yeah, so that’s a great point, too. So one of the things is I gather, you might have some hormonal imbalances, right? So in disruption, so for example, the precursor right of proteolysis, which is protein breakdown, is cortisol. So this is one of the parameters of biomarkers that we see in athletes who have very high levels of cortisol. It’s a hormone that responds to both psychological and physiological stress. So when an athlete is not mentally stressed, but you see very high levels of cortisol, that athletes is breaking down more Protein, that normal probably. And then you look at the anabolic side of it, which is testosterone. So you look at the ratio. And many times you see athletes with very low testosterone levels, because they have to keep replenishing, replenishing the catabolic effects, right of cortisol and lack of energy while training. So that’s where you you start getting that catabolic profile of the athletes. And that takes them to a different layer, which is more inflammation, right? So the inflammation that we see when when you have muscle breakdown, you end up with muscle micro tears and muscle damage. Not saying there’s an injury, right, but you can see muscle damage and there are multiple research studies on these right for decades, with muscle biopsies, looking at disruptions in the muscle structure. But we can we can see this in blood analysis and biomarkers. And the thing is, too is that the physiological mechanism to repair or one of the physiological mechanisms to repair muscles is inflammation, right. And inflammation also brings usually water retention, liquid retention. So this is one of the times also where the cyclists are trying to eat less. And then they get muscle breakdown and they get catabolic, and they end up gaining more weight. And a big part of that weight is liquid, right. And they say, I gained three pounds or six pounds. So how in the world I’m eating a lot less Yeah, but you have inflammation, low grade inflammation, and particularly in the Boulder area. As we know, people tend to be really hardcore when it comes to nutrition and training. And we see a lot of people with muscle damage, and especially in the age groupers, right. That’s something that caught my attention people in their 40s, 50s, 60s they have a lot of muscle damage chronically. And we still don’t know what the consequences could be about this, because normally historically, we haven’t seen this is the first time in in humans where we see people in their 60s, 70s training and doing marathons, the regular base, right, but they have low grade chronic inflammation. Now, we know from medical research, and then pretty much logical studies that chronic low grade inflammation can can lead to multiple diseases. So this is an area where I’m particularly concerned and then the other endocrine responses that we see is like thyroid function. So we know that this is the thing like I used to see before coming to Colorado, especially maybe one people a year are diagnosed with hypothyroidism. Now in Colorado, you see, and other places in the country. Sure, I’m just you know, because we’re in Colorado, we we see hardcore athletes all the time, right. But I, I’ve been seeing once a week and the men’s majority of these people, they do not have hypothyroidism and explanation is these they are really tired really to pick for months, and they’re dragging their feet, and they’re finally go to their doctors and they do a blood analysis and part of the regular panels that are done of chemistry panels is TSH, which is cheap to do. And then TSH chose, it’s a little bit elevated. But in the in the low high end right of TSH. And so therefore, the doctor says, Okay, there’s like, chronic fatigue, which is a sign of hypothyroidism and their high levels of TSH. Bingo! So that athlete in many occasions leaves that doctor’s office with a prescription with for thyroid medication. And when you have thyroid medication, you typically, people start using maybe 15 minutes 25 to 50 micrograms, and they’re still feeling good, but it’s artificial. It’s like if you’re tired and fatigue and you have a gallon of coffee, you’re going to feel good. But eventually you’re going to develop resistance. And this is where many of these people they they start with 50 micrograms 75, 100, 125. And when they get to those levels, that the firing function is gone and there’s nothing you can do. So they have to be on medication for the rest of their lives, where they never needed to be on that medication in the first place. So one of the things that I’ve been trying to do at the School of Medicine and trying to talk to several in the chronology is working with fire areas, right, he’s like, whenever you see someone with that profile, who’s an athlete or active individual who’s chronically fatigued and tired, and slightly elevated TSH levels, please do more farther analysis looking at the three four antibodies, you know that they really can give you the whole picture and the majority of the cases they do not have hypothyroidism. So anyway, this is another but there’s a disruption in the endocrine system where TSH produces a little bit more than normal and any my fullview thinking that you find you have hypothyroidism, which you don’t have,
Trevor Connor 19:50
The problem is most doctors wouldn’t know to look for that and I can share an example of an athlete that you know, this was not a story that ended well who experienced it. She was a talented marathon runner, but she had only been running for two years. So she was still early in her career and she got hold of the training plan from a friend who was an Olympic Marathon Runner, and just jumped right into that level of training, which was way too much for I had a chance to talk with her because she was getting ready for one of her big events and she was just fatigued, and doing what a lot of inexperienced athletes were doing, saying, I’m not performing very well, I need to increase my training. I need to train harder and I was talking about going, you know, I had a couple conversations. I was like, that’s not the issue. The issue is you are overreaching, pushing overtraining right now and convinced her to take a couple of weeks off, and she was terrified. But she she felt she had no choice. So she did that a couple of weeks before her event and then I had her do a very gradual getting back of the legs before the event and just because she went into that marathon rested. She had her best performance ever, but then basically said problem solved. Thank you went back to doing that Olympic training plan and she is, as you just said, she’s now on thyroid medication for the rest of her life.
Dr. San Milan 21:11
Oh no, yeah, that’s unfortunate. Because yeah, there are many cases like that and I think like, so yeah. So it’s great that you guys are bringing up these subject thank you for doing that. Because I really think that among all of us involved in this space, right, we need to kind of raise awareness both for athletes as well as for providers right so this could be a serious problem down the road and, then we really need to make sure that this is well diagnosed before someone is put on thyroid medication.
Trevor Connor 21:41
Right and I’ll also bring awareness to another problem that a lot of people probably aren’t aware of. So you were talking about that inflammation. I went snowshoeing a couple of weekends ago, and I hadn’t snowshoed in about five months, or a while since basically last year and I planned an hour, took a wrong route ended up doing over two hours and the next day, my legs were so swollen, there was so much water in my legs. I was getting made fun of at work because my pants kept going riding up my legs and it looked like that five sizes too short for me. So we need to inform people this there’s another side effect. Another problem that a lot of people aren’t aware of your pants are gonna look bad.
Dr. San Milan 22:19
Yeah, exactly. And absolutely. And then so yeah, and if it’s in your case, right, it’s cute, right? But we see, you know, people who are chronically in that situation, and I don’t think that that can be good and we know already from epidemiological studies that low grade inflammation is usually related to develop in different diseases, right? So it’s good to be in that situation and also what I want to point out is like a substrate or an imbalance, also, that is very typical to like we know very well that when you have muscle damage, you cannot store glycogen correctly. So that’s going to create an extra big problem. And in addition, which is going to add more fire to that that vicious cycle, right overtraining, where, where that person now finally starts, okay, now I have to eat more carbohydrates, right, and starts eating more carbohydrates, but there’s a lot of muscle damage, so you cannot store glycogen properly. It’s like trying to grab water with your hands, right and we don’t know exactly the mechanisms of why, when there’s muscle damage, you cannot store glycogen properly. But until you do not repair your muscle fibers or micro tears, you’re not going to fully restore glycogen. So again, this is this is more recent to be preventive through proper monitoring, right and be hand to hand with nutrition and, and I never get tired of saying this right that nutrition and training, they must go hand to hand.
Dr. Jason Gladney Explains a Clinical Approach to the Issue of Recovery
Trevor Connor 23:52
It’s critical for all of us, pro or amateur to monitor a recovery so we don’t slip into an overtrained state. I asked Dr. Jason Gladney from a clinical perspective, what are some of the most important markers that athletes need to pay attention to?
Dr. Jason Gladney 24:07
I think, you know, some of it can be boiled down to, you know, subjective things that they can listen for you what I do, when I get out of bed, as I take, take an assessment of how I’m feeling usually is pretty stiff and sore, and about 10 minutes later is feeling a little bit better. But those heavy legs, those things that you can kind of feel when you’re taking those first steps in the morning. You know, that’s an important sign thing that you can kind of look at, I think it’s wise to actually monitor your vitals at home. You can see what your resting heart rate is in the morning. You know, sometimes that’s a prelude to some type of overtraining mildly. So we call it like functional overreach, if it’s a short term thing, but also looking at hydration status. When I’m training hard, I’d like to get on the scale frequently. So you can kind of know get a good idea of what your fluid status is, unless you’re trying to lose weight and you’re expecting the numbers to keep going down. You Wanna try to maintain body weight and doing it after rides to is quite important, you can get a better idea of how much fluid you lost out there and physiology, we think losing about 2% of your fluid, or plasma volume is probably okay, anything above 4%, there’s gonna actually going to be quite a detriment to your performance, it seems. So those are probably some of the more important things to do. Usually, in these high level athletes, they’re hyper aware of what their bodies feel like. And I think that has played a big role in keeping them out of trouble. We see a lot of athletes and it’s kind of become more and more common to hear about athletes like Calve this year who had a reactivation of epstein barr, and just the amount of time that he lost as a result of it, we tend to get in the situation, when you’re feeling good, you want to do more race more train harder. It’s the thing that you got to listen to your coach and listen to kind of that inner voice, and you’re telling me is probably not a good idea to do this. I see people every other injury that comes in, they said, I was feeling great. And I kept pushing and pushing. And now this happened. So just keep that in mind. And I think learning to be subjective about how you’re really feeling, taking stock and in things every day, I think that plays a huge role with keeping you out of trouble.
Trevor Connor 26:09
So if you’re going out for a ride, or if an athlete is going out for the ride, are there any particular signs that they have those you would say, turn around, go home, or talk to your coach or go see a medical doctor,
Dr. Jason Gladney 26:20
I think the biggest rides that that plays in is if you have intensity on your schedule, and I’ll tell my patients that you’re going out there and you’re doing some of the first reps on the set and boys just not coming around. You’re really struggling to hit your numbers. That’s not the time to try to push through it. I think yeah, kind of stop the set. Just been easy. Go home, take a break, eat rest. See how you feel the next day? Talk to your coach, if you do have one and kind of see what they suggest. Is it something that it was a key workout that you got to make up? Or is it one of these ones, it wasn’t that big of a deal that you can skip it this week and meanwhile, recover and feel good and fresh for the next round?
Dr. San Millán Discusses How Physical and Psychological Stress Factors Can Alter a Catabolic State
Trevor Connor 26:59
I think you brought up a really important point earlier on when you talked about the cortisol response, which puts you in that catabolic state you said that stress causes cortisol release and we’re talking both physical and psychological stress and you know study that that had a big impact on me when I was doing some research on overreaching. Looking at right now it’s monitoring the athletes training response subjective self reported measures trumped commonly used objective measures and suddenly it really caught me in this study as they basically said some of these tests of your mood state so your rescue your MTDS, pick up overtraining before a lot of these objective measures showing just how that mood state, the mental side how important that is. And as you point out, recreational riders might not put in a lot of hours, but they might have a lot of work and life stress that’s gonna have an impact.
Dr. San Milan 27:50
Absolutely. Exactly. And yeah, then how many times I’ve seen a blot analysis and someone’s cortisol levels are off the chart, right? And obviously, the first thing is, oh, my God, you’re training too much, right? And like, and then you start seeing, like, no, actually, this person is not training more than five hours a week or so. But then you see, like, Whoa, that person is going through enormous mental stress, or maybe some events, right, they go through some drama, you know, or some, you know, traumatic situation their lives know, are stressful day. Yeah, sure that that that alone, you know, it’s going to take cortisol off the chart and is going to interfere with recovery with the anabolic catabolic balance, right? And therefore, yeah, you’re have a lot more chances to become overtraining.
Rob Pickels 28:34
So Dr. San Milan, we’ve really covered the high level and we fully understand that overtraining is a big issue for a lot of people, both at the amateur and at the professional level, but how do we even know when overtraining or overreaching or any of this imbalance is occurring?
Dr. San Milan 28:51
Yeah, that’s a great point and this is what we we need obviously, as many scientific methods to deploy, but also we can be creative. So, to really describe an earlier like that goes mood state test, you know an indirect parameter that already been given some information right, but then we have a whole wealth of refineries out there that we can deploy. So obviously blot analysis and we can discuss that more in depth later, but broader analysis are going to be this tremendous amount of information, right but we also have also, you know, multiple other parameters like looking at your training peaks for example. Now you can see workload if you if you have some experience coaching you can you can really see that that athlete is not completing training completely so for example training piece for me is my Bible, and I have no conflict of interest, right. I don’t have any financial relationship with any business like it’s been a wonderful tool right and transformative right for cycling, you know, and triathlon and running them. Hopefully they keep growing, you know, sports too. So one thing I look at the training and one of the key things that used or seen is our heart rate, heart rate is it’s a true physiological parameter. And it’s been kind of forgotten, always coming back. But I still remember about a decade ago or a little bit more like people didn’t want to know anything about heart rate. I vividly remember that and I’m sure Rob, you were, because we were talking about the while back, right? It would Trevor, the same thing, right is like how people just trained by watts, and then in the heart rate was old school, and didn’t mean anything, right. But fortunately, heart rate is back. And now we know everything about hurry variability, as a big concept, etc. Right. But that one thing that I see right away is like, you know, the heart rate response to exercise. Either cyclists have today, for example, intervals, likely press or, you know, or FTP. And we know that those power up, let’s put a number, let’s say 300 Watts, the heart rate normally is, let’s say 180 beats per minute. And today, the heart rate is 165. And that athletes telling you, man, My heart doesn’t get up. That’s a sign of fatigue. Yeah, right there, they you can see right in the spot without the need of broader analysis, just looking at the data. So yeah, so one of the things that I do every morning, I just look at the data from 2015, from the athletes on the team, you know, in UAE, for example. And, and that’s where I started identifying things like this, and I contact them, and I tell them the Hey, you know, how do you feel like yeah, today, my heart did not respond to that. And that’s where you start concluding that fact, there are issues, right? Although times is that the athlete, himself or herself who contacts you, right? And tells you, hey, there’s something wrong, my heart doesn’t get up, don’t have good legs, good sensations. So I always tell them listen to your heart. And this is a very powerful parameter. They have old I’ve used for a long time, since I was a cyclist. Since I was 15 years old, I was using heart rate for this. And he’s been very helpful for me. So with heart rates against the true physiological parameter, so you know when to break down glycogen into glucose, you need colonies. And these are indispensable because that does one of the main major triggers for the breakdown of glycogen into glucose for energy purposes. So the body has about about 500 grams roughly can be more or less on glycogen. That’s how we store glucose, right? The brain alone uses about 125 grams a day, that’s a normal brain. So then you will be left with about 375 grams, let’s say you have 500 grams total. But if you’re if you have a very stressful life, or very highly mentally mental activity all day, yeah, your brain is going to utilize more glucose or maybe twice, and therefore your glycogen storage is going to be lower. Anyways, the important thing with these is that the body is very wise and the brain is very white and the brain senses that there’s not enough glycogen in the body. So the brain in a way tells the legs. Hey, look, I don’t care much about your legs. You know, I’m the boss. I’m the sheriff. And I need the glucose right? So I don’t want you to break down so much glucose. I don’t want you to shut down completely glycogen breakdown and same thing for to the liver, right? I don’t want you to shut down completely because we all die especially means that the brain right? But I want you to break down less glycogen, right? And this is where we also capture in the metabolic testing with athletes. So an athlete who has learned glycogen may be oxidized in 2.5 grams, for example, at a given intensity, but now it’s oxidation. 1.5 grams for one gram. So what drives that is like a decrease in correct glycogen breakdown rate. And that’s true by decreasing catecholamines. Well, guess what activates the heart catecholamines, the famous adrenaline and noradrenaline, right? And this is what we may not see that at rest, but especially we see that high exercise intensities were because of those lower secretion of catecholamines to protect right our blood breakdown of glycogen into glucose. That’s a collateral effect, the heart activation is going to be lower. So this is why it’s always very important to listen to your heart. And this is a sign when the heart doesn’t get up normally, and it’s like 8, 7, 10 beats per minute lower and higher. firts Absolutely. That’s a sign of glycogen depletion or lower glycogen levels.
Armando Mastracci Explains His Understanding of How Strain Plays a Part in Recovery
Trevor Connor 34:35
Both Dr. Sol Milan and I are old school believers in checking your resting heart rate. But I had a chance to talk with Armando Mastracci, the developer of Exert trading software, his thoughts on those metrics, and whether the software can effectively analyze your recovery state.
Armando Mastracci 34:51
You know, I believe that up until this point, a lot of the coaches and more enthusiasts have been using the existing metrics and trying to interpret them to understand how much acute training load and chronic training load, and try to understand, you know what kind of recovery demands they might have as a result of those, but it requires lots of interpretation. Part of that is because of the differences that you’re going to see in results from individual to individual. So within exert because we’re a little more precise in terms of identifying strain, because we’re identifying across multiple dimensions that we can start to identify recovery in a more generalized way. So the user, the athlete doesn’t necessarily need to understand all of the ways in which the numbers and how to interpret the numbers, we now interpret them for the user. So one of the things you’ll notice within the software is that when you first log in, you’ll see a number of stars on your on your training, we call this training status. And what we what we do is we combine two dimensions that you would normally get from your PMC, or in our case, what’s called the XXPMC, which is your chronic training load, acute training load is an interpretation of that information for you automatically. So we show you essentially what your training load is we show you rather than as a number, we give you a star. So people talk about I want to get to my third star, I want to get to my four star, and all that really means is that they want to accumulate more training load. So we give them a so it becomes more motivational, rather than chasing a number is to say, Okay, I’m chasing a certain level, right? And we associate level three as being a competitive athlete, where you get to reach a certain level of training most you’ll see that with a number of stars, but then we color code stars as well, to let you know whether what’s the software? What’s the data showing about how you should be feeling, right. So if you just came off, you know, big, multiple rides over the weekend, they’ll turn red, right, you’ll show it’ll show you as being very tired. And we a lot of questions saying Yes, surely I’m very tired, but I’m not very tired. Thank you, we always have to explain. It’s just what the data is expressing about you, you know, the data can’t know how you feel, it can only say what the data says about how you feel. And we do characterize it in terms to try and match how we expect them to feel. Because then it kind of makes sense, say, Oh, if it says I’m very tired, you know, the software is gonna prescribe recovery, this is going to, let’s say, give you a couple of days before it’ll prescribe additional training. And these become easy visuals for people to interpret and to follow. So this is kind of how we believe the software can come in, is to give an interpretation of what the data says about an individual, and help them identify how they, you know, we’re really what how they should be treating their recovery. Again, anybody can do whatever they feel like at the time, but at least the software is giving them some level of interpretation of the information.
Trevor Connor 37:33
So it sounds like the software is using things like the the acute training load to say, hey, you just hit yourself a lot of training that’s beyond what you normally do, right? So you might be getting fatigued right now. But it’s indirect measures at the end of the day.
Armando Mastracci 37:49
It’s indirect, right. And we can certainly look to incorporate and there’s a desire to do this was to incorporate incorporate HRV. So if we start collecting HRV data is heart rate variability, right, which is another in durability. So actually some of our users that are actually doing that actively monitoring the HRV corresponding with the day that they get from our system. So there is there is a risk of a relationship. In fact, going back to Tonya Churchill, she actually did an assessment where she compared the the recovery demands with a recovery index from HRV. And she found you know, that they’re directly related. So it’s kind of interesting, we can certainly do that, something very similar.
A Brief Message from Rob
Rob Pickels 38:32
Tis the season for spring knee, as March sunshine and early Spring weather inspires us to ramp up our riding mileage, our knees don’t always keep up. If you’ve got knee pain, we have the solution for you. Fast Talk Lab members can follow our new knee health pathway featuring our new Director of Sports Medicine, Dr. Andy Pruitt, see the introduction to the Knee Health Pathway at fasttalklabs.com.
How to Monitor Your Heart Rate Through Your Recovery
Trevor Connor 39:00
What I find really interesting, you know, I’m very big on telling athletes, you need to use heart rate, you need to use power, you need to use rate of perceived exertion, you can’t just do intervals, lock it in a given wattage and think that you you’re executing perfectly. And I tell them about this lowered heart rate. And I always find it interesting when athletes see that I tend to get one or two responses. One is what you see that’s why heart rates useless because I was 170 last week at that wattage and this week goes 163. So heart rates give me bad data as opposed to going well, I’m fatigued. Likewise, I’ll have athletes that will go to do their intervals with their heart rates low and then destroy themselves to get that heart rate up. Instead of what I find athletes really struggle with is seeing that low heart rate and going maybe I shouldn’t be doing my intervals today.
Dr. San Milan 39:51
Exactly. And that’s what I tell us it’s always listen to your heart and any of the heart it doesn’t get up today. The best training day today is turned around and go home, recover, pile up on carbohydrates, and you will still have tomorrow you do it again, the training you postpone into tomorrow, and you’re going to feel much better. And in fact, you feel it. And the seeing of doing this with the heart rate is that if you listen to the heart every day, even on top of it, right, if you’ve never listened to the heart, you keep pushing it, as you said, pushing and pushing. And that’s where you get to worse situation. Right. But I think it’s very important. And another thing I’d like to point out about the heartbeat is also the resting heart rate in the morning. This is, again, I’ve been using since I since I was 15 years old, and call me old school if you want to. But I think that this was like a maybe of the first concepts that me and others, like, you know, we’re doing, you know, back in the day, so heart rate variability, I know that that the definition of high variability has changed now and is a little bit more complicated. And now we have fancy software’s and etc. But the other day, you know, like a very simple looking at the heart rate, as we have discussed with high intensity efforts. That’s a hurry variability from one day to another, right. But also, there’s another way of high variability in the mornings. So let’s say that your heart rate in the morning when you wake up, and you don’t need to put a heart monitor on you can just, you know, like count through your pools right in your wrist and count the 15 and multiply it by four or kind of fomented, you want to write, but let’s say your beats per minute, which usually are quite constant, let’s say that you’re like 50. And, and tomorrow, you’re 49. And there’s a 48 and 52, you’re within, you know, within a very narrow range. And that’s the way most of the times is, but let’s suppose that one day you wake up and you’re 65, right, that’s not normal, right? Because it’s a deviation. It’s a variability right from the normalcy. And that means something, there’s something physiological, again, we have to remember, right, that heart rate is a truly physiological parameter, and it’s responding to something. And so that they could be that you’re not simulating the training correctly. And maybe you haven’t recovered from the day before, or sometimes your incubating a virus and how many times I’ve told this to athletes, like, man, because they seem to be many times you see, in fact that they haven’t recovered completely. So okay, you know, today, we’re going to take it easy, but other times like then, you know, you’re recovering well, but you might be creating a virus, like, What are you talking about? Yeah, well, three days later, two days later, boom, they come down with a with a cold or flu. And, you know, this is this is a pre COVID. Right? But anyways, this is an indicative and then. So that’s the thing when people start using these methodologies as well, the best way like what if you wake up with a heart rate that is significantly elevated to what he usually is, okay, maybe you can go out there and train, but go with all the radars fun, right, and listen to every single movement that you do. And normally, yeah, if you have bad sensations that day, something is out of whack, you’re going through something, either not recovering or incubating a virus or something of that same chain, turn around, go home, and recover. And maybe the next day, you still are high, or maybe the next day, boom, you’re back to 50. And that’s where you can resume training. So heart rate in the morning, it’s a very useful parameter. I have used it with elite athletes all these years, and I still do
Rob Pickels 43:24
Doctor San Milan, I love this holistic approach that you have, right? Because then we can get this really great depth and understanding of what’s happening inside of somebody. How do we take that holistic approach and begin looking at blood biomarkers? How much more information can we get about an athlete from the various things that we can look at derived from the blood?
Dr. San Milan 43:45
Yeah, so there are multiple biomarkers, as you very well know, right? So one thing that I look at, within biomarkers, there’s other holistic approaches, right? So I look at the overall thing. So one of the first things that I look at are oxygen carrying capacity, biomarkers, right, so and the one that I look at hemoglobin, so one gram of hemoglobin transports 1.34 milliliters of oxygen, right? So if you have a drop of only one gram of hemoglobin, your oxygen carrying capacity is going to decrease somewhere between 6 to 7%. Right? So that, you know might not be a performance killer, but maybe could, right could be and is definitely going to decrease your performance. So we have to pay attention to that right? The oxygen carrying capacity. At the end of the day when people come to altitude here to Colorado or, or the Italian Alps or Sierra Nevada, in Spain or whatever the whole purpose is to increase hemoglobin, right oxygen carrying capacity because obviously it’s a huge advantage. So if you decrease it, because you’re over trained, that’s when now your oxygen carrying capacity is going to be jeopardized. And so this is one biomarker and we can get into why people decreased their hemoglobin but yeah, that’s one biomarker.
Rob Pickels 45:04
I do want to dig into that one a little bit deeper, because it’s the question that I had as you were speaking. And I’m sure that it’s the question that the listeners have, we know that the hemoglobin decrease is going to decrease performance. But how is that related to overtraining? What are the mechanisms? You know, if we’re using it as a biomarker? What are the mechanisms that are causing it to come down when the athlete is doing too much or not recovering enough?
Dr. San Milan 45:29
Yeah, exactly. So it is a sign that the body’s not adapting correctly, right. It is a sign of that. So this is this is one of the eternal discussions that I have with many nutritionists, right, where they look at hemoglobin and are decreasing in red blood cells. And right away, they say, Oh, this is an iron deficiency issues, right? When No, it is not necessarily now, deficiency issues, because you can see that they’re their ferritin levels, which is how we store iron. They’re completely normal. Right? So this is why it’s not narrow deficiency issue. And it’s a no training issue. And that’s something that is sometimes again, this is where we it’s important to work with nutritionists who now something right about physiology and metabolism and training because it’s easier for them to understand concepts like this right? And the importance of that, because if people take, oh, it’s the typical thing, oh, you need to take iron if you take iron and it doesn’t do absolutely anything. And this is something that no we need to make sure that we understand these concepts in a more holistic manner.
The Importance of Hemoglobin
Rob Pickels 46:36
Dr. San Milan, when we’re having low hemoglobin, we’re having low red blood cells in the athlete. Is that because they’re not making enough? Is it because their red blood cells are dying, what’s leading to this low hemoglobin in the overtrained person?
Dr. San Milan 46:50
So yeah, so every day we destroyed 200 billion would be red blood cells is the former cells in the body red blood cells have the highest turnover. So we destroyed 200 billion red blood cells, we need to replace them. So when I always say that the red blood cell is the taxi of the oxygen, but within the red blood cell, the hemoglobin is this the actual seat where the oxygen sits by and so to assemble, hemoglobin, you need iron. And you need vitamin D 12, and folic acid as well as the red blood cells, too. So, you know, that’s what I was saying immediately. Many, many nutritionists or many doctors too, they see a decrease in hemoglobin or red blood cells. And they right Oh, wow, that this is a non issue. So they are getting iron. But But no, you might have plenty of iron, it is just you’re not producing enough red blood cells and this is where you get into the whole anabolic catabolic situation. So to produce a red blood cell, anything that is producing a cell in the body where is like to repair a muscle damage or to produce more muscle or to produce a red blood cell. That’s an anabolic process, right? EPO, right? It’s an anabolic hormone in in the sense that it creates new red blood cells, right. So if your status is prevalently catabolic status, all the anabolic processes are going to be suppressed. So one of them is erythropoiesis, which is red blood cell production. So this is why many times we see athletes whose red blood cells are going down, or hemoglobin is going down. And yet their ferritin levels, which is the way we start iron ore, the iron levels themselves are completely normal. So this is where we can pinpoint and really identify that the issue is not iron or nutrition in this case, is overtraining. And there’s a prevalence in that catabolic status of an athlete.
Coach Jeff Winkler Discusses Biomarkers in The Recovery Process
Trevor Connor 48:45
We asked coach Jeff Winkler, if there are any biomarkers of recovery that he uses with his athletes?
Jeff Winkler 48:52
The answer is, yes, I have a bit of sensitivity to iron deficiency, because it’s something I experienced when I was racing. And it was a very difficult problem, because the medical community kind of didn’t buy it and so getting us doctors to address it. It was like pulling teeth. I couldn’t convince them that there was any performance impact to iron deficiency. But I can tell you experientially, it was dramatic. There was times when I got iron shots and it was, it was like 180-degree turnaround. I went from being your boss that you can’t get out of your own way. And I lost contracts. Because of that, you know, where the season kind of just fell apart. And I was like, I don’t know what’s going on. I’m training Well, I’m not doing anything wrong and now I can’t perform in the race, it took years to really get on top of it but I remember there was occasions where I received you know, an iron injection, which was really the only way to deal with the problem with it quickly, and it flipped me and my performance just resumed where it seemed like it should have been all along. And so, based on my experience I paid you know, I, especially at CU, because these were, many of the kids who were on that team were quite talented. And you could see them start to struggle, and there was no cause, like, you could look at school, you could look at the whole stress, picture you everything, and you’re like, there’s really no reason why you shouldn’t be performing better. And they believe this too. And I would encourage blood test to check iron status, and probably 75% of them were iron deficient, you were or at least borderline. So that’s one that I pay close attention to, I think, you know, in elevation, you don’t, I mean, I haven’t worked with anyone that has like true anemia. But the female athletes that I have worked with that that problem is even more acute than with men, but it’s a real thing for the men too. So that’s my focus, I guess from a blood perspective.
Dr San Milan Discusses the Impact Muscle Damage Can Have on Recovery
Trevor Connor 50:56
Obviously, hemoglobin is a great thing to look at to see what’s going on with the athlete. But there are other good biomarkers, and one that I have a particular interest in is biomarkers of muscle damage. Now, I’ll point out that some sports you see more muscle tearing than other sports that are high and have a lot of eccentric activity, you’re gonna have more tearing, cycling, you’re gonna see less because there is no eccentric movement, but I still think you’re gonna see some muscle damage in cycling. So can you talk to the sort of biomarkers that you have for muscle damage?
Dr. San Milan 51:29
Yeah, you’re absolutely right. That yeah, other sports, you know, they have more eccentric movements, like, you know, soccer, football, basketball, right? Team sports in general. Right? And in fact, you know, not only they have more muscle damage, but in fact, they have more muscle tissue injuries, and especially in the, in the hamstrings, right? Is the muscle that goes the most. But yeah, you’re writing cycling, we don’t we don’t have those kind of movements. Eccentric nearly as much. Right but you used to see important muscle damage. So this is what we look for. So we look for like other two main enzymes that I look for. There are CK or Cpk Creatine Phosphokinase or Creatine Kinase, or in also LDHA, or LDH, right? Lactate Dehydrogenase. So those are enzymes. They’re normal in the in the metabolic function of muscle cells. But when they’re micro tears, they leak to the bloodstream. And that’s where we can identify them. And we know that they come from the muscle, this is something that has been done also for decades in cardiology, right? This is nothing new. I mean, I’ve been doing this for 26 years, but a cardiologist had been doing for a century or so. So because the heart is it’s a muscle, and when there’s like a myocardial infarction or heart attack, yeah, there’s like, damage to those muscles. And that’s where you see very high levels of CK and LDH. Obviously, you’re not going to see this in your regular athletes. So when you see that those levels are high, they’re coming from the muscle, right and this may be due to excessive training and poor recovery, as we discussed earlier, you can elicit muscle damage by, for example, having low carbohydrate availability, because if you run out of glycogen, the body has an evolutionary mechanism where it’s going to utilize muscle protein, right to produce energy. So the muscles first are breaking themselves to feed themselves. And that’s where you have micro tears. And that’s where you’re going to see muscle damage is very common. And that’s something that we have seen also in in ICU patients. So ICU patients, they pretty much all they have at some point, muscle waste or Achestia. And you have a lot of muscle damage in these patients. Now, they’re not exercising, but they’re run out of glycogen as well. And this is a study that we published looking at glycogen content, but yeah, the muscles are eating themselves to feed themselves and especially glutamine. It’s a huge fuel for the cells. And the biggest largest pool of glutamine is the skeletal muscle. So that’s why you see these patients who are in the bed, at the ICU with a very tremendous amount of muscle damage without doing anything, and it’s because of lack of proper nutrition. So anyway, this is why we can also see it in athletes that is not just the exertion or the eccentric movement itself, but could be also the nutrition.
Rob Pickels 54:19
Now for some clarification, anytime we do activity, anytime we do training, we’re going to have a little bit of inflammation in the muscle that stays localized. Right. And I think that the levels that you’re talking about are when we’re starting to detect these in a systemic when we take blood out of your arm. We’re seeing these increases in CK and LDH and other markers. Is that correct?
Dr. San Milan 54:40
Yeah, exactly. And this is something that I use also to dial in training, because sometimes Yeah, you’re right. It’s a slight elevation. It’s physiological and it means that yeah, that there’s that stress that you were seeking with training is there and this is where okay, now we need to really pay attention to the second phase of the training which is recovery nutrition as we discussed, and it’s no big deal, you know, all the time is the opposite, you see that you believe that that athlete is training well, but has absolutely no stress, you don’t see any single blood parameter that is showing any stress. So that means that that athlete is either being too conservative or maybe the training workload can tolerate more. And that’s quite individual, you know, there are people who would the same hours or training workload some people get it can get muscle damage, and overtraining, other ones, it can hold a lot more. So this is what this is something that I used to dial in trainings better, you know, all the time, which has been in altitude training, for example now and yeah, just everybody’s responses, as you guys know, is different in altitude. And you see a lot of muscle damage in altitude, the parties because you utilize a lot more carbohydrates out to to the rest. So you really need to pure lab and some people respond better than others. But I use these plot analysis to dial in training quite a bit.
Trevor Connor 56:01
So something I found really interesting. There’s a fairly recent study. This is a 2021 study called recovery, stress response of blood based biomarkers. And they looked at a more chronic under recovered state in soccer players and badminton players. And they found three markers that seemed to be elevated in this this non recovered state one, as you just talked about was creatine kinase, aisle six, which makes sense because aisle six helps to regulate that muscle repair process. But the one that really surprised me was IL 17, which is released by a particular T cell called th17 cells, which their job is to fight off bacterial infection. So you want to know, why would they be elevated here though, we did talk about this inflammatory process and muscle repair in a previous episode and talked about in many ways, if that repair process that inflammation gets in a normal state kept localized, but if it gets to be too much, it can become systemic, and it can mimic in many ways. sepsis, which is a influx of too much bacterial overload into your body. So this was really interesting to me. And particularly, it goes back to what you were saying before about this inflammation being damaging, you know, my thesis research was looking at inflammation and its effects, particularly autoimmune disease. But doing that research, what I really saw is if you have chronic elevation of th 17, that precedes autoimmune disease that precedes heart disease that precedes some cancers. So really surprising here to see IL 17. In this mix.
Dr. San Milan 57:37
Yeah that’s interesting. Yeah. It’s pretty inflammatory. element. And yeah, it’s involved in in, you know, in autoimmune disease is it’s increased right, in different diseases. And one of them is are arthritis right. Rheumatoid arthritis which is, tends to be quite common, right. In many former elite athletes right. Now. I’m not an orthopedic specialist. Right. But could that be due to the excess wear and tear of the joints? Or could be that in combination also, with the chronic right, IL 17, you know, in these athletes, leading to arthritis down the road, because it’s quite prevalent, you know, in, especially in team sports. But yeah, you’re right. I think that, yeah, I don’t think that kind of to what we were saying at the beginning, right. You don’t want to have a lot of chronic low grade inflammation, right. And you have aisle six and aisle 17, that if you’re chronically high levels, like, you know, I don’t think we have a lot of chronological studies. But I personally don’t think it can be good. Down the road, right?
Trevor Connor 58:39
Oh, I agree completely.
Dr. San Milan 58:41
And this is also I don’t know if this is, but I mean, we’re seeing that more the longevity of athletes is longer and longer. And I think that that deployment of science and the understanding from the workload to calculate from the nutrition from the monitoring is highly contributing to this longevity, because before athletes, they didn’t have much numbers, they didn’t have much data. And it was typical to see athletes in the low 30s. To say, Okay, this is this is good, my body can continue. I stopped now. You see athletes were peaking in their low 30s. Right, and they’re well in shape and feel that close to 40. You know, so this is something I think that is changing significantly.
How to Maintain Longevity with Your Vitals
Rob Pickels 59:26
When we talk about athlete longevity, I think something that we know changes with age is endocrine changes, right? And how does the endocrine system play into biomarkers? As we’re trying to assess an athlete, right? We have cortisol, we have testosterone, what do we need to know about those to make good decisions?
Dr. San Milan 59:47
Yeah, that’s a very good question, too. And, and I’ve seen that because of, yeah, we are going to see more data in the coming years, I guess, because we’re seeing more deployment of this methodology. He is ready to really get a lot of parameters and insert establishing correlations with aging. Right. But I think that going back to the same thing, as we age, obviously, especially men will produce less testosterone, women produce less estrogen. You know, we see lower levels for growth hormone as well released. And so we tend to get more in a catabolic mode faster by so this is what I think that for aging athletes is more important even to monitor the status. And this is why probably why, as I mentioned earlier, especially in age groupers, I see tremendous amount of muscle damage in this population and catabolic states could that be that, sure that catabolic, you know, like machinery is as expressed as in younger individuals, but the anabolic machinery is not leading them to that imbalance. But I think that it’s important to monitor athletes are really mean recreational athletes for said, who are aging and understand these better and, and we see that testosterone, as you point pointed out, right, it’s a great biomarker for an embolism and decreases. But yeah, we need to make sure that I would say that those ones were engaging, you know, like, in levels of irregular activity, and they do some blood analysis here and there to make sure that everything is in place is checked.
Rob Pickels 1:01:20
So if we take a step back and look at the wider picture of that, then we can use these biomarkers of testosterone and cortisol to get a sense of the balance of anabolic and catabolic processes in all ages, not just in the aging athlete, correct?
Dr. San Milan 1:01:36
Oh, absolutely. Yeah, exactly. Yeah, this is a great indicator, you know, like testosterone and anabolic marker. And cortisol is the catabolic marker. And both are really, we use this all the time to understand his balance with all kinds of athletes. Right? But absolutely, you know, the whole ratio is it’s quite important to see if there’s, you know, as I said, sometimes, we see very high levels of cortisol and very low levels of testosterone. So that athlete is it’s in a very catabolic, so performance, normally, it’s going to be decreased. And that the athlete has also a higher possibility of getting injured. Sometimes we see a very high levels of cortisol, but also very high levels of testosterone as well. So there’s a balance, right, there’s a lot of catabolism. But at the same time, there’s a lot of anomalies in there in some times, you know, like, as I mentioned earlier, like, we may see very, very low levels of cortisol, and very high levels of testosterone. So that is telling us that athlete can be pushed more, because he’s not, you know, can tolerate a lot more work load. This is another parameter that I use, when I see these ratios like, wow, this athlete is not getting much stimulation, you know, you can tolerate more for sure. And when it comes for females is more difficult to tolerate this ratio is because of the testosterone in women, right? But at least cortisol is always good, a very good parameter. Overall, it’s more difficult to do this and women and I tend to do then a growth hormone levels or IGF 1, which are very expensive to do and not easy to find, right, but that the testosterone to cortisol ratio in female athletes, it’s more difficult, obviously. So then we might have more like our cortisol levels, and then holistically approach but your heart rate when you call a high intensity is where your sensations know your perceived effort. So this is trickier. Definitely working with female athletes. Yeah, because of the their physiological responses also to their menstrual cycle, right? It can, it can be more difficult to figure out some parameters that can lead us to some conclusions.
Trevor Connor 1:03:51
A really good point.
Rob Pickels 1:03:52
How does the individual athlete utilize this? Do they have to work with their doctor or their services? How often should people be testing it? Is this just something that we do? Because maybe it’s expensive when something is going wrong? What’s the actual actionable info that comes out of this?
Dr. San Milan 1:04:09
Oh, that’s, that’s a great, great question. Great point, for sure. So I normally obviously, with elite athletes, I do this on a monthly basis, even less than times. But I think that we’re for more like a recreational athlete, or even like a competitve athlete that’s not a professional, I will do that. Definitely a baseline at the beginning of the preseason, to see where your baseline levels are. So you can go back to them right. I will do another one. Maybe when the season starts, or in the first part of the season, maybe another one in the middle of the season. And anytime that you feel that something out of whack, or something is wrong, my performance has decreased has plummeted. Or maybe like a month before my main goal or a month and a half, where you can see that things have changed and they’re leading you towards overtraining. And you can correct those so I would say death And you know, like a few times a year, that will be important to do. But regarding like, yeah, where to go, this is this is the difficulty, especially here in the United States in Europe. You know, there’s a lot of future of doing these blood biomarkers, I was doing this when I was 15 years old as a junior, they were normal thing for kids. Now, when I came to the US, 13 years ago, almost nobody in the country did this. And in fact, within our sports medicine fellowship at the university, you know, people don’t do this either people in most sports medicine doctors here are more into their orthopedic side, it’s not as holistic as in Europe or in Europe, more of the sports medicine doctor is also a physiologist, nutritionist / Cardiology is a little bit of everything. It’s a much more holistic. And I think that more and more sports medicine doctors are getting into that route two to become more holistic. Right. But it’s not easy. And I don’t have the answer for that. And your family doctor or your primary care provider. Yeah, they’re very busy enough already with with dealing with people with important diseases, right, that they don’t have much time to look into this are they don’t have that education or experience? Right. But so yeah, it’s not easy. So I would, I would try to find out about some some providers, someone who has access to these broader analysis, and has some experience. But again, it’s not easy. I don’t have the right answer, to be honest of where to go,
Rob Pickels 1:06:34
Yeah, sometimes recognizing it’s a tough problem to solve is the right answer. And, you know, maybe this is a Fast Talk Labs project for the future.
Episode Take-Away’s
Trevor Connor 1:06:43
There we go. Well, I mean, I’m sure this is gonna become increasingly important. And hopefully, this is something that doctors are going to be able to start doing for athletes, as opposed to, as you said, just focusing on biomarkers for when somebody is in a disease state. So I think it’s time Dr. San Milan, thank you. That was very informative. But it’s time to jump into our take home. So you know, the routine here you have one minute, give us what you think is the most pertinent message that our listeners need to take away from this episode.
Dr. San Milan 1:07:12
Great. Well, first of all, thank you very much, Trevor. And, and Rob, I really appreciate this, I think this is a very important topic. And the work that you guys are doing to educate our listeners and open their eyes and new doors is fantastic and instrumental. So yeah, great work. And thank you for doing this. And so as a quick take home, I would say that, as I mentioned, like nutrition is key to prevent overtraining and nutrition and training has to they have to be together, then monitoring different parameters. Some, obviously, the blood analysis are more difficult to do. But there are other ones there. They’re quite easy, inexpensive, which is, as we have discussed the heart rate response when we wake up, when we exercise, this is a very reliable parameter, incredibly reliable. And then yeah, listen to your sensations. That’s the thing, too, you know, like, if you feel that you’re tired or fatigued, maybe you’re tired and fatigue, and maybe you have to understand that you don’t have to train much even even if you if you only are training six hours a week, but and then try to work on the things around why your particularly tired, so if that the nutrition is the lack of sleep, is the lack of recovery. And also seek some help a viewer into some goal or you want to train at a more specific level, try to run yourself by people with experience understanding this these issues.
Trevor Connor 1:08:37
Fantastic. Rob, your first one from this side?
Rob Pickels 1:08:40
Wow, Trevor, my take home from this, what I’m hearing is strengthening the things that I have believed for a long time that a holistic approach is absolutely critical for everything that we do. And we can include blood biomarkers in that both blood biomarkers need to be looked at holistic themselves, but also as part of a holistic package that’s assessing an athlete, there’s a lot of things that we can dive into it is perhaps a difficult topic for people to be able to follow along with this because a lot of it is is very detailed information and that, you know right now the medical community in the US is maybe a step behind on really a great thing or a real benefit to athletes. And you know, so there will continue pushing that the athletes have this as a resource. There are other resources and you can continue to arm yourself with knowledge in the attempt to get better at what you do.
Trevor Connor 1:09:32
So my take home I really latched on to that comment you had in your chapter about the fact that too many athletes see a recovery day as a missed opportunity. There is this mentality of of I might be feeling bad and the legs might be hurting but I got to be tough. I got to just push through because that’s what athletes do. But talking about these markers talking about the effects, you see that it is more than that. If you are constantly pushing through and not recovering. Your body goes into a catabolic state, which means it can’t be rebuilding tissue, it’s depleting your your energy stores, you’re seeing inflammation and surprising forms of inflammation that if that’s kept elevated can lead to bad places which lead to conditions so that arrest is a missed opportunity is really the wrong mindset. You need to find that balance. You need to let all these things that are happening inside your body, get to the places they need to get to, you need to get to that anabolic state, you need to restore those fuels and clear that inflammation and that’s why the recovery is so important.
Trevor Connor 1:10:36
All right, Dr. San Milan thank you so much. It’s always a pleasure having you on the show. – Thank you so much. –
Trevor Connor 1:10:42
That was another episode of fast talk subscribe to Fast Talk wherever you prefer to find your favorite podcast. Be sure to leave us a rating and a review. The thoughts and opinions expressed on Fast Talk are those are the individual. As always, we’d love your feedback. Join the conversation at forums.fasttalklabs.com to discuss each and every episode. Become a member of Fast Talk Laboratories at fasttalklabs.com/join To become a part of our education and coaching community. For Dr. Inigo San Milan, Dr. Jason Gladney, Armando Mastracci, Jeff Winkler and Robert Pickels. I’m Trevor Connor. Thanks for listening.